Herniated disc of the thoracic spine - prolapse of the intervertebral disc of the thoracic vertebra (ICD-10 M51). It is characterized by pain, impaired sensitivity of the skin and somatic disorders. The diagnosis is made on the basis of a set of data: the results of examination of organs and systems to exclude pathologies due to other reasons, and MRI. Discs of the lower thoracic vertebrae (Th8-Th12) are mainly affected.
Treatment is conservative and operative. Hernia of the shmorl of the thoracic spine is a hernial bulging in the body of the above or below the vertebra due to rupture of the cartilaginous tissue of the intervertebral disc. No surgical treatment is required.
The reasons
The etiology of this pathology is based on processes that lead to the appearance of cracks and a decrease in the strength of the annulus fibrosus:
- sedentary lifestyle;
- long-term static and static-dynamic loads of significant intensity;
- trauma;
- osteochondrosis of the thoracic spine;
- dysmetabolic disorders;
- autoimmune diseases.
Evolution of hernial protrusion
In their development, prolapses go through several stages:
- The marginal protrusion of the disc up to 1-5 mm with the preservation of the outer layer of the annulus fibrosus. It is called protrusion.
- Extrusion or formed hernia with a violation of the integrity of the ring and bulging of 5-8 mm.
- Sequestration is characterized by aseptic necrosis and detachment of hernia tissues (the size of which often exceeds 8 mm), followed by their migration in the spinal canal, which is fraught with disabling complications.
According to the degree of narrowing of the spinal canal, hernial protrusions are divided into small (0-10%), medium (10-20%) and large (> 20%).
Symptoms and differential diagnosis
They are determined by the behavior of the hernia, its localization and the degree of protrusion. This can be compression of the roots of the spinal nerves or the substance of the spinal cord. Based on topographic criteria, protrusion is:
- lateral,
- ventral (represents the least danger);
- central (median or posterior), the most dangerous for its complications;
- paramedian.
Some neurosurgeons distinguish dorsal, median (as a variant of dorsal evolution), circular, ventral, and foraminal localizations.
In relation to the parts of the spine - the upper, middle and lower thoracic.
Also:
- With a central location, compression of the spinal cord is observed, accompanied by the development of compression myelopathy with the appearance of lower spastic mono- or papararesis, as well as pelvic disorders.
- With lateral localization, the symptom complex of compression of the spinal roots with manifestation of disorders comes out on top:
- sensory perception in the chest;
- somatic innervation when a hernia affects the visceral branches, which causes functional changes in the work of internal organs.
Hernia location (department) | Symptom complex | Differential diagnosis |
| Upper thoracic (Th1-Th4) | Thoracalgia, paresthesia in the upper chest and interscapular region; paresthesia and weakness in the hands, numbness of the hands (Th1-Th2); difficulty swallowing, disturbances in the peristalsis of the esophagus. | Angina pectoris. |
| Middle thoracic (Th5-Th8) | Shingles like intercostal neuralgia; difficulty breathing; gastralgia, dyspepsia; disturbances in the work of the pancreas, leading to pathological changes in the metabolism of carbohydrates. | Herpes zoster (herpes zoster type 1). |
| Lower thoracic (Th9-Th12) | Pain in the kidneys, under the ribs, in the upper abdomen, intestinal dyskinesia (Th11-Th12), abnormalities in the functioning of the pelvic organs. | Acute abdomen, appendicitis, acute cholecystitis, acute pancreatitis. |
Difficulties in diagnosis are caused by the specificity of the symptoms of the disease. The protrusion, depending on the location, is able to mimic the signs of thoracic and abdominal diseases. Therefore, to verify the diagnosis, a neurologist can involve specialized specialists.

© Alexandr Mitiuc - stock.adobe.com. Schematic representation of the location of the hernia in the thoracic spine.
Tests with Nitroglycerin or Corvalol can help to distinguish disc prolapse from the manifestation of a symptom complex of angina pectoris, in which the pain caused by compression of the nerve roots will not be stopped.
When carrying out the differential diagnosis of discogenic pathogenesis (disc protrusion) with diseases of the gastrointestinal tract, it should be borne in mind that pain in the abdomen is in no way associated with food intake.
Symptoms may differ in women and men. The latter may have decreased libido and erectile dysfunction. Women are susceptible to ovarian pathology, menstrual irregularities, which leads to a decrease in the possibility of conception, pain in the areolar region, which are often confused with the onset of mastitis (breast infection).
Diagnostics
Diagnosis is based on:
- typical patient complaints (segmental disturbances in the sensitive and motor spheres, pathological changes in the work of internal organs, innervated by the compressed nerve trunk);
- data of neurological examination and clinical picture of the disease;
- MRI results (with direct contraindications, for example, the presence of an artificial pacemaker, CT of the spine can be used, but the accuracy of the study is inferior to MRI);
- data from laboratory studies, instrumental diagnostics and consultations of related specialists, allowing for differential diagnosis (to help verify a hernia and exclude exertional angina will help a detailed history collection, ECG data and functional tests showing the absence of myocardial ischemia).
Difficulties in making a diagnosis can be due to intercurrent diseases. The patient may be bothered by thoracalgia and with diagnosed exertional angina on the background of the existing prolapse in the thoracic spine. Also, a hernia can provoke an attack of angina pectoris.
The tactics of treatment can be determined by two specialists - a neurologist and a therapist (or cardiologist).
Treatment
It is subdivided into conservative and surgical. Conservative therapy is carried out in inpatient and home conditions, providing for measures aimed at:
- elimination or reduction of thoracalgia;
- prevention of protrusion growth.
Drug therapy
Includes appointment:
- NSAIDs (Naproxen, Ibuprofen, Celecoxib, Ketoprofen, Carprofen, etc.);
- corticosteroids (metipred);
- local blockades (anesthetics + corticosteroids);
- muscle relaxants with severe spastic syndrome (Tolperisone, Mydocalm, Sirdalud);
- chondroprotectors (Glucosamine, Aorta - are used to improve the trophism of the nucleus pulposus, they demonstrate maximum efficiency at the stage of protrusion of the intervertebral disc);
- B vitamins (B1 and B6, stimulating the restoration of nerve fibers).
The drug approach allows you to stop the pain syndrome and create a favorable background for the use of other conservative treatment methods.
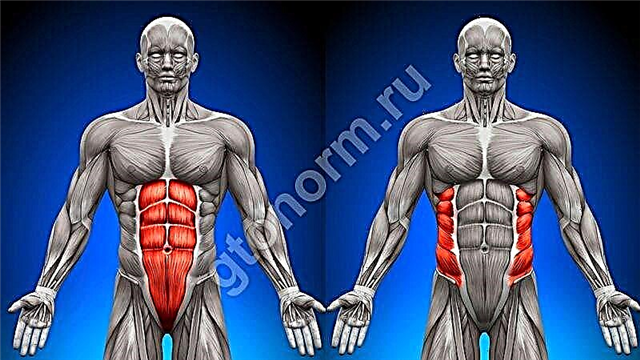
The effect of gymnastic exercises (exercise therapy)
Therapeutic gymnastics helps to increase blood supply, relieve spasms and form a muscle corset, which helps to relieve the musculoskeletal system. Exercises for a hernia of the thoracic spine are prescribed strictly on an individual basis during remission, more often at an early stage of the disease, or during the postoperative recovery period. Exercise therapy in the first stages is carried out under the supervision of an instructor in the gym. The recommended sets of exercises can then be performed at home.
Acupuncture, reflexology
They are used to relieve pain and muscle tension.
Manual therapy and spinal traction
They are used to increase the distance between the vertebral bodies.

© Mulderphoto - stock.adobe.com. Stretching the spine.
Impact of massage
Massage is prescribed to relieve the increased tone of the paravertebral muscles. It is used to relax and improve blood supply in the early stages of the disease in the remission phase.
Physiotherapy
It is used to provide muscle relaxant and anti-inflammatory effect at all stages of hernia evolution during remission. Used: hydrocortisone ultraphonophoresis, electrophoresis, magnetotherapy and UHF.
In the absence of the effect of conservative therapy and / or the appearance of signs of myelopathy, they resort to surgical treatment.
The positive effect of ERT after operations at the early recovery stage (sessions of EHF, laser and magnetic therapy, electromyostimulation) has been clinically proven.
Professor Bubnovsky's technique
Dr. Bubnovsky recommends a set of exercises focused on stretching the back muscles:
- Standing straight and placing your feet shoulder-width apart, you need to smoothly perform forward bends, trying to stick your head and hands between your knees.

- Putting your straightened leg on the back of the chair, you should try to lay your body on the thigh while exhaling, trying to grab the sock with your hands.

- Lying on your stomach, stretch your arms forward, lifting the body and pushing off the floor as you exhale.

- In a standing position, stretch upward, trying to rise on your toes as high as possible.

Surgery
It is indicated when the conservative approach is ineffective for 6 months. The approach includes:
- laminotomy or laminectomy - complete or partial resection of the vertebral arch for decompression of the vertebral canal; often combined with fusion - fixation of adjacent vertebrae for fusion;
- laminoplasty - a tomia of the vertebral arch in order to increase the space around the roots and create a hinge;
- disc extirpation (microdiscectomy (as an option - endoscopic), discectomy).
After surgical treatment, complications are possible:
- infectious - myelitis, spinal arachnoiditis;
- non-infectious:
- early - bleeding, alteration of spinal nerves or dura mater;
- late - the formation of ankylosis (fusion) of the bodies of adjacent vertebrae.
Sports for prolapse of the thoracic spine (permitted and prohibited sports)
Sports activities are limited. Permitted types include:
- aqua aerobics and swimming (as therapeutic and preventive measures):
- the muscles relax, the load on the spine is reduced, the ligaments and joints are strengthened;
- strengthening the respiratory system, improving blood supply.
- workouts in the gym under the supervision of an exercise therapy instructor;
- Pilates;
- push ups;
- fitness and yoga classes;
- exercise with simulators;
- sitting on a fitball;
- hanging on the horizontal bar;
- Cycling at a leisurely pace;
- squats (during remission).
Any of the above exercises must be performed only under the supervision of a specialist. Workouts that require sitting or standing should be excluded:
- weightlifting;
- high and long jumps;
- football, basketball, rugby, skiing;
- race walking;
- power sports.
Complications and consequences of prolapse
The progression of nosology can lead to:
- pronounced intercostal neuralgia;
- spinal cord compression alteration (one of the most dangerous consequences):
- paresis of the limbs;
- complete loss of functions of the pelvic organs.
- disturbances in the work of the heart and respiratory organs (pains in the chest and interruptions in the work of the heart are felt; shortness of breath occurs, it becomes difficult to breathe);
- the progression of orthopedic disorders (scoliosis, kyphosis);
- the formation of intervertebral hernias in other parts of the spine - due to pathological redistribution of loads and exacerbation of the disease.
Due to a violation of innervation, feedback from one or another visceral organ suffers. The system of its autonomous regulation is destroyed. Colon dyskinesia can evolve into colitis, and functional disorders of the pancreas can transform into pancreatitis. Moreover, prolapse can lead to life-threatening disorders of the cardiovascular system (acute myocardial infarction; exertional angina and unstable angina; sudden cardiac arrest).
Prevention
The risk group includes representatives of those specialties and occupations that involve prolonged static and static-dynamic loads on the spine: surgeons, athletes, salespeople, office workers.
It is much easier to prevent the formation of a hernia than to treat it. Exercising every day will help you avoid it. Various movements contribute not only to the production of synovial fluid and hydration of the discs, but also to strengthen the deep muscles of the back, which reduces the load on the spine.
When doing preventive exercise, it is important to remember that:
- The discs are better suited to vertical loads than to horizontal or oblique loads. This means that when lifting a heavy object, you should squat, but not bend over.
- Carrying out sedentary work, it is necessary to change the position of the body several times a day, performing preventive exercises, try to sit as little as possible.
- Swimming and water aerobics are extremely useful in preventive terms, as they allow you to strengthen the muscle corset, while simultaneously relieving the spine.