Sports injuries
1K 0 03/22/2019 (last revision: 07/01/2019)
Rupture of the meniscus of the knee joint is a violation of the integrity of the special cartilage inside the joint of the same name, which acts as a pad and shock absorber.
General information
Menisci are cartilaginous structures localized within the knee joint, between the articular surfaces of the femur and tibia. Formed mainly by fibers of special collagen. By percentage:
- collagen - 65 ± 5%;
- extracellular matrix proteins - 10 ± 3%;
- elastin - 0.6 ± 0.05%.
Inside each cartilage formation is a red zone - an area with blood vessels.
Allocate the outer and inner meniscus. Each is subdivided into a body, front and rear horns. They act as natural shock absorbers, distributing significant loads and contact stress and stabilizing the joint during rotation. Meniscus injury is a common pathology in people aged 17-42 who are active or do hard work. The left and right knee joints are damaged at the same frequency. Ruptures of the medial meniscus occur 3 times more often than the lateral. Alterations of both menisci are extremely rare. Men are injured more often than women. Treatment is conservative or operative.

© joshya - stock.adobe.com
Etiology
The causes of injury are due to mechanical stress. May be accompanied by ligamentary stretching or tearing. Most often they are:
- The combined effect, consisting in a sharp rotation of the lower leg:
- inward - leads to alteration of the external meniscus;
- outward - to rupture of the internal cartilage formation.
- Excessive flexion or extension of the joint, or abrupt abduction or adduction.
- Running on uneven ground with excessive body weight.
- Direct injury - a fall with a knee bump on a step.
Frequent injuries provoke the development of chronic inflammation and degenerative processes in the cartilage tissue, which increases the risk of re-trauma.
The causes of cartilage degeneration, which increase the likelihood of traumatic damage, also include:
- infectious diseases - rheumatism, brucellosis;
- repetitive microtrauma in football players, basketball players, hockey players;
- chronic intoxication with benzene, formaldehyde, vinyl chloride;
- metabolic disorders - gout;
- malfunctions of the endocrine system (imbalance of growth hormone, estrogen and corticosteroids);
- congenital pathologies (hypoplasia of cartilage tissue, menisci, vessels of the knee joints; congenital ligamentary insufficiency).
After 40 years, degenerative processes are the most common cause of the named pathology (menisci lose strength and become more susceptible to traumatic effects).
Considering the above, a number of authors conditionally divides meniscus tears into:
- traumatic;
- degenerative (manifest when performing habitual movements or minimal loads, the clinical picture is erased).
Classifications of alterations and their degrees
Damage is complete or partial, with or without displacement, in the body, or in the anterior or posterior horn. Taking into account the shape, the breaks are divided into:
- longitudinal;
- horizontal;
- radial;
- by the type of "watering can handle";
- patchwork;
- patchwork horizontal.
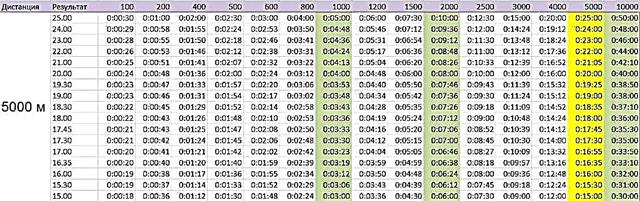
Conventionally, according to MRI data, four degrees of alteration are distinguished:
| Power | Characteristics of meniscus damage |
| 0 | No changes. |
| 1 | Inside the inter-articular joint there is a tear of the cartilaginous tissue, which does not affect the outer shell and is determined on MRI. There are no clinical symptoms. |
| 2 | Structural changes extend deep into the meniscus without affecting the outer shell. |
| 3 | A complete or partial rupture of the outer shell is determined. Puffiness against the background of severe pain syndrome makes it easy to diagnose. |
Symptoms
The signs of pathology differ depending on its period, as well as on the severity of the damage.
| Period of injury | Clinical picture |
| Acute | Nonspecific symptoms of inflammation predominate (pronounced edema; local aching pain and limitation of movement, especially extension). Hemarthrosis is possible (with trauma to the red zone). |
| Subacute | It develops 2-3 weeks after injury. The severity of inflammation decreases. Local pains, joint capsule induration and limitation of movement prevail. With alteration of the medial meniscus, flexion is more often difficult, lateral - extension. The manifestation of pain occurs under certain conditions, for example, when climbing stairs (during the descent, it may be absent). Due to the detachment of a fragment of the meniscus, the joint may jam. Usually, rupture of the posterior horn leads to limitation of flexion, and the body and anterior horn to extension. |
| Chronic | Constant moderate pain and limitation of movement are typical. |
Which specialist to contact
You should consult a surgeon or an orthopedic traumatologist.
Diagnostics
The diagnosis is made on the basis of anamnesis (the fact of injury), examination data (with surgical tests), patient complaints and the results of instrumental research methods.
You can confirm the diagnosis with:
- X-ray, allowing to identify damage (the study can be carried out with contrast); the value of the study in excluding possible fractures of bone structures;
- MRI, which is characterized by significantly higher accuracy compared to radiography;
- CT, less informative than MRI, is used when the latter is impossible;
- Ultrasound, which provides an opportunity to identify and assess the degree of damage to the connective tissue structures;
- arthroscopy, providing the opportunity:
- visualize trauma;
- remove damaged fragments of cartilage;
- introduce medications.
Treatment
It is multi-stage. It is selected individually.
In the acute period are shown:
- puncture of the articular bag and suction of blood, if any;
- rest and immobilization of the leg with significant alteration on the recommendation of the attending physician (plaster cast can be used); with an insignificant radial or medial rupture of the horn, complete immobilization is not indicated due to the risk of contractures (a pressure bandage from an elastic bandage is used);
- taking painkillers (Ibuprofen, Ketanol, Diclofenac);
- movement with crutches in order to minimize the load on the damaged joint;
- on the day of injury - locally cold, give the leg an elevated position.
Further appointed:
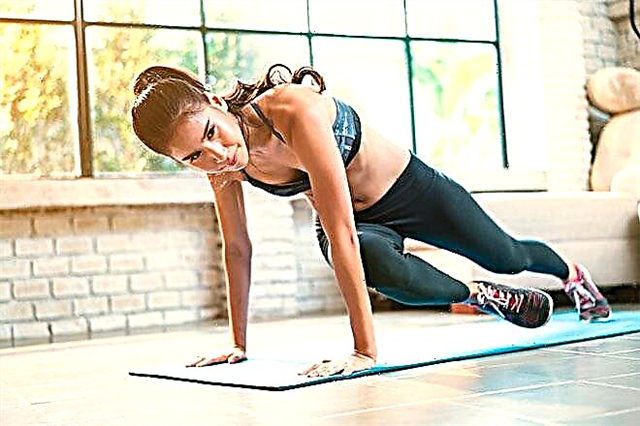
- Exercise therapy;
- massage;
- physiotherapy (UHF therapy, microwave therapy, laser, magnetotherapy, hydrotherapy, electromyostimulation, ultrasound exposure, hirudotherapy, electrophoresis);
- chondroprotectors (glucosamine, chondroitin sulfate).

© Photographee.eu - stock.adobe.com. Exercise therapy.
Surgical intervention is resorted to if diagnosed:
- detachment of the body and horns of the meniscus (more often there is a rupture of the posterior horn of the medial meniscus, accompanied by a crunch during squats);
- rupture of the meniscus with its subsequent displacement;
- crushing the meniscus;
- lack of results from conservative therapy.
The most widespread are meniscectomy and meniscus-preserving surgery through suture and special structures. Access to damaged tissues is carried out using an open method or using an arthroscope.
Plastic surgery is possible in case of separation from the joint capsule or longitudinal and peripheral vertical ruptures. The chances of success are higher with a fresh injury and a patient under 40 years of age.

© romaset - stock.adobe.com
Meniscus transplantation is used for complete destruction of cartilage tissue. The grafts are lyophilized or irradiated menisci. There is literature data on the development of artificial grafts.
The average duration of the operation is approximately 2 hours.
The prognosis worsens when a large fragment is torn off or cartilage degeneration has begun - absolute indications for meniscus extrusion.
Exercise therapy
In order to prevent hypotrophy of leg muscles, strengthen the ligamentous apparatus and stabilize the menisci, exercise therapy is indicated. Charging should be done several times a day. The duration of the exercise can be 20-30 minutes.
| Exercise type | Description | Photo exercise |
| Squeezing the ball | You need to stand with your back to the wall, holding the ball between your knees. You should sit down slowly, bending your knees. |  |
| Step | One foot is placed on the platform, the other remains on the floor. The position of the feet should be changed one by one. |  |
| Stretch | The injured leg is bent at the knee, the foot is wound behind the back, and then smoothly lowers to the floor. |  |
| Swing with resistance | Holding on to the support with your hands, the sore leg starts up on the healthy one alternately from different sides. |  |
Recommendations of S.M. Bubnovsky
The recommended exercises are divided into simple and difficult:
- Simple. The crushed ice is wrapped in a cloth that wraps around the knees. You should move on your knees, gradually increasing the number of steps to 15. After removing the ice, kneel down and try to lower your buttocks to your heels, gradually increasing the sitting time to 5 minutes (at the beginning, you can put a mat under the buttocks). Then stretch your legs forward, grabbing one of the feet with your hands and pulling it up.

- Complex:
- Squats. Knees at a 90 ° angle. The back is straight. Don't bend over. It is allowed to use a support. Dr. Bubnovsky recommends doing 20 squats in one approach. There should be at least 5 approaches per day.

- Get on your knees, stretch your arms in front of you. Lower down, touching the floor with the buttocks.

- Lying on your stomach, clasp your ankles, pulling your feet to your buttocks, touching them with your heels.

- Lying on your back, stretch your arms along your torso and bend your knees in turn. Without lifting your heels off the floor, pull them up to your buttocks, helping yourself with your hands.

Rehabilitation and military service
At the stage of rehabilitation after surgery, it is recommended to limit the load on the knee joint for 6-12 months. Depending on the characteristics of the operation performed, different schemes of exercise therapy, ERT and massage can be used. Among the medicines, NSAIDs and chondroprotectors are prescribed.
If the conscript injured the meniscus before conscription, a six-month delay is allowed for treatment. Instability leads to exemption from military service:
- knee joint 2-3 degrees;
- with dislocations at least 3 times in 12 months;
- diagnosed in special ways.
Serving in the military requires a complete recovery from the consequences of injury.