Post-traumatic arthrosis is a progressive degenerative-dystrophic change in a joint of a chronic course that occurs as a result of exposure to a traumatic agent.
The reasons
Even minor damage can provoke the development of degenerative processes in the joint. The causes of post-traumatic arthrosis of the knee joint include:
- pathology of the anatomical structure of the joint;
- displacement of fragments;
- damage to the capsular-ligamentous structures;
- untimely or inadequate therapy;
- prolonged immobilization;
- surgical treatment of knee joint disorders.
Most often, this pathology occurs due to:
- violations of the conformity of articular surfaces;
- a significant decrease in the blood supply to various elements of the knee joint;
- prolonged artificial immobilization.
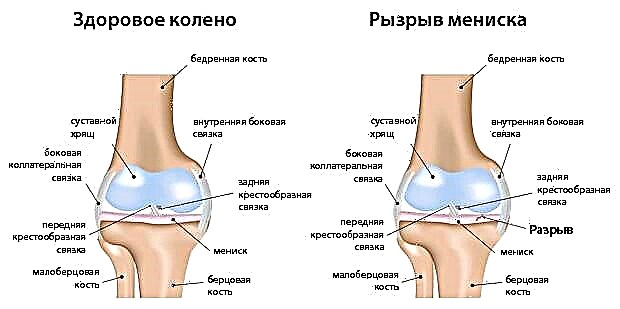
The reasons for the development of arthrosis can be intra-articular fractures with displacement and injuries to the menisci and ligaments (for example, rupture).
© joshya - stock.adobe.com
Stages
Depending on the degree of manifestation, three stages of pathology are distinguished:
- I - painful sensations arise during physical exertion, with movements of the affected limb, a crunch is heard in the joint. There are no visual changes in the joint area. Pain occurs on palpation.
- II - pronounced pain during the transition from static to dynamics, limited movement in the morning, stiffness, intense crunching in the joint. Palpation determines the deformation of the joint space with uneven areas along the contour.
- III - the shape of the joint is changed, the pain becomes intense even at rest. Painful sensations intensify at night. There is limited movement. The damaged joint is sensitive to changes in weather conditions.
Kinds
Depending on the localization, several types of post-traumatic arthrosis are distinguished, each of which will be described below.
Post-traumatic arthrosis of the knee joint
The inflammatory process covers cartilage, muscles, ligaments and other elements of the joint. The average age of patients is 55 years.
Post-traumatic arthrosis of the shoulder joint
The disease can affect one or both of the shoulder joints. The causes of this pathology are their displacement and stretching.
Post-traumatic arthrosis of the fingers
When the cartilage tissue of the joints of the fingers is damaged, a degenerative-inflammatory process develops.
Post-traumatic arthrosis of the ankle
This pathology occurs due to displacement and cracks.
Post-traumatic arthrosis of the hip joint
The reasons for the development of this type of disease are ligament rupture and other joint damage.
Post-traumatic arthrosis of the elbow joint
Injuries lead to a deterioration in the condition of the elbow joint. Complex injuries can cause extensive damage to the cartilage and deformity of the elbow, as a result of which tissue wear is accelerated and the mechanics of the joint are disrupted.
Symptoms
Pathology can be asymptomatic for some time or hide behind the background of residual effects after joint injury. With an advanced stage of the disease, clinical symptoms of arthrosis can be observed for a long period.
In the initial stages, the disease manifests itself:
- pain;
- crunch.
Pain syndrome is characterized by the following features:
- localization in the damaged area of tissue;
- there is no irradiation;
- aching and pulling;
- initially insignificant painful sensations become more intense with movements;
- at rest, they are absent and arise during movement.
The crunch increases as the disease progresses. It refers to the stable symptoms of post-traumatic arthrosis. At the same time, the nature of pain is changing. They spread throughout the knee joint and can radiate above or below the knee. The pain takes on a twisting, stable character and becomes more intense.
Significant symptoms for post-traumatic arthrosis of the knee joint are the appearance of pain and stiffness when coming out of a state of rest. These signs make it possible to preliminarily diagnose the disease even without using other research methods. Most often they appear after sleep.
In the future, with the progression of pathology, they join:
- swelling of adjacent soft tissues;
- muscle spasm;
- deformation of the joint;
- lameness;
- deterioration of the emotional and psychological state of the patient due to constant pain syndrome.
Diagnostics
Disease recognition is carried out based on clinical symptoms, patient complaints and anamnesis. The doctor should certainly clarify whether there were any joint injuries in the patient's past. With a history of trauma, the likelihood of post-traumatic arthrosis increases significantly.
The diagnosis is confirmed after examination of the patient and palpation of the damaged area. An overview X-ray of the joint is performed. In some cases, MRI or CT is prescribed to clarify the diagnosis.

© Olesia Bilkei - stock.adobe.com. MRI
When taking X-ray, the picture of the disease is as follows:
- I - narrowing of the joint space, along the edges of which bone growths are located. There are local areas of cartilage ossification.
- II - an increase in the size of bone growths, a more intense narrowing of the joint space. The emergence of subchondral sclerosis of the end plate.
- III - intense deformation and hardening of the cartilaginous surfaces of the joint. Subchondral necrosis is present. The joint gap is not visualized.
Treatment
The disease requires complex treatment. At the mild stage, drug therapy is used in combination with exercise therapy and physiotherapy. If conservative treatment does not lead to the desired effect and the pathology progresses, surgical intervention is performed.
The goal of therapy is to prevent the destruction of cartilage tissue, relieve pain, restore joint functionality and improve the patient's quality of life.
Drug therapy
For post-traumatic arthrosis, the following drugs are recommended:
- Chondroprotectors. They prevent cartilage destruction and have a protective effect on the matrix.
- Metabolism correctors. They contain vitamin and mineral complexes and nutrients.
- NSAID drugs. Reduces pain and inflammation. The drugs are used during an exacerbation of the disease.
- Hyaluronic acid.
- Medicines to improve microcirculation in the affected area.
- Glucocorticosteroids. Prescribed in the absence of the effect of drug therapy.
- Means for external use (ointments, gels) based on components of plant and animal origin.
Physiotherapy
Complex therapy is used to improve metabolic processes in cartilage tissue, relieve pain and slow down the destruction of the joint.
Physiotherapeutic treatment methods:
- Ultrasound therapy;
- inductothermy;
- electrophoresis;
- magnetotherapy;
- ozokerite and paraffin wax applications;
- phonophoresis;
- local barotherapy;
- bifoshite treatment;
- acupuncture;
- balneotherapy.

© auremar - stock.adobe.com
Surgical intervention
With the progression of arthrosis, despite conservative treatment and if indicated, the doctor may prescribe surgical treatment.
The following surgical methods are used:
- endoprosthetics;
- plastic ligaments;
- arthroplasty of the joint;
- synovectomy;
- corrective osteotomy;
- arthroscopic manipulation.
The operation is only one of the stages of treatment and does not allow to completely get rid of the pathology.
Folk remedies
Traditional medicine recipes are used as an adjunct to primary treatment. Their use is most effective at the initial stage of the disease or for its prevention.
St. John's wort, burdock, nettle and other plants are used as anti-inflammatory, decongestant and regenerating agents. They are used for the preparation of tinctures, decoctions, ointments and other products for internal and external use.
Complications
As a result of the progression of post-traumatic arthrosis, ankylosis, subluxation and joint contracture can occur.
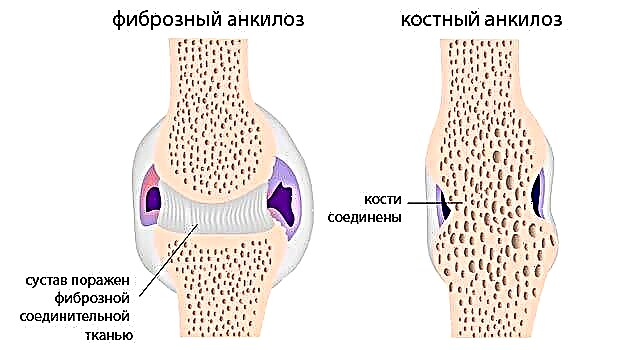
© Alila-Medical-Media - stock.adobe.com
Forecast and prevention
The outcome of the disease depends on the severity and adequacy of treatment. In some cases, complete restoration of the joint is not possible. Ideal cure is a rather rare option, there are almost always minimal residual effects.
Destroyed areas of cartilaginous tissue cannot be restored. The main goal of therapy is to stop the progression of the disease. Late seeking medical help, neglect of the process and the elderly age of the patient can worsen the prognosis of the course of the pathology.