A knee injury for an athlete is a very unpleasant and very painful thing. It is she who can knock out even the most professional and hardened athlete from the training process for a long time. Some eminent and promising athletes at one time had to leave the big sport precisely because of the injury to this joint. How to avoid a knee injury and what to do if it does occur, we will tell in this article.
Knee anatomy
The bone base of the knee joint is made up of the distal end of the femur, the proximal end of the tibia, and the head of the fibula. The articulating surfaces of the bones - the head of the femur and tibia - are covered with thick cartilage. The immediate places of "contact" of the bones are called condyles. They are curved at the femur and, conversely, concave at the tibia. To increase the congruence of the articulating surfaces, as well as for a more uniform pressure of the condyles on each other, there are cartilaginous formations - menisci - between the articulating surfaces of the bones. There are two of them - internal and external, respectively medial and lateral. The whole structure is reinforced from the inside with a system of ligaments.

© toricheks - stock.adobe.com
Ligamentous apparatus
The cruciate ligaments pass between the menisci - the anterior and posterior ones, connecting the femur to the tibia. They play the role of restraining mechanisms: the anterior cruciate ligament prevents the shin from moving forward, the posterior one from shifting the shin back. Looking ahead, we note that the anterior cruciate ligament is more susceptible to injury.
On the front surface of the joint, the menisci are fastened by the transverse ligament of the knee joint. The joint capsule has significant dimensions, however, it is rather thin and does not have significant strength. It is provided by the ligaments surrounding the knee joint:
- tibial ligament - runs from the head of the tibia to the medial condyle of the femur;
- peroneal ligament - runs from the head of the fibula to the lateral condyle of the femur;
- oblique popliteal ligament - makes up the back of the articular bag of the knee joint, partly is a continuation of the hamstring muscle tendon;
- tendon of the quadriceps femoris muscle - runs along the front surface of the knee joint, attaches to the tuberosity of the tibia. The patella is also intertwined here - a small sesamoid bone, designed to increase the power potential of the quadriceps. The part of the tendon that runs from the patella to the tuberosity is called the patellar ligament.

© Axel Kock - stock.adobe.com
The inner surface of the joint is lined with a synovial membrane. The latter forms a series of extensions filled with adipose tissue and synovial fluid. They increase the internal cavity of the knee joint, creating some additional cushioning reserve along with the menisci.
The tendons of the muscles surrounding it give additional stability to the knee joint. These are the muscles of the thigh and lower leg.
Anterior muscle group
When talking about the muscles of the thigh, they can be divided into four groups, depending on their location in relation to the knee joint.
The anterior group is represented by the quadriceps femoris muscle. It is a massive formation, consisting of four heads that perform different functions:
- the rectus femoris extends the thigh;
- the medial, lateral and middle heads of the quadriceps are combined into a common tendon and are the extensors of the lower leg;
Thus, the function of the quadriceps is twofold: on the one hand, it flexes the thigh, on the other, it unbends the lower leg.
The sartorius muscle also belongs to the muscles of the anterior thigh group. It is the longest in the body and runs through the hip and knee joints. Its distal end is attached to the tuberosity of the tibia. The function of this muscle is to flex the hip and flex the lower leg. She is also responsible for supination of the hip, that is, for turning the latter outward.

© mikiradic - stock.adobe.com
Posterior muscle group
The posterior muscle group includes muscles whose function is to extend the hip and flex the lower leg. It:
- biceps femoris, she is the hamstring. Its functions are listed above. The distal end attaches to the head of the fibula. This muscle also supines the lower leg;
- semimembranous muscle - the distal tendon attaches to the subarticular edge of the medial condyle of the tibia, and also gives the tendon to the oblique popliteal ligament and the popliteal fascia. The function of this muscle is flexion of the lower leg, extension of the thigh, pronation of the lower leg;
- the semitendinosus muscle of the thigh, which is attached with the distal end to the tuberosity of the tibia and is located medially. It performs the functions of flexion of the lower leg and its pronation.
Inner and lateral group
The inner thigh muscle group performs the function of adducting the thigh. It includes:
- the thin muscle of the thigh - distally attached to the tuberosity of the tibia, is responsible for adduction of the thigh and its flexion at the knee joint;
- adductor magnus - is attached with the distal end to the medial epicondyle of the femur and is the main adductor muscle of the thigh.
The lateral muscle group, represented by the fascia lata tensor, is responsible for abducting the thigh to the side. In this case, the tendon of the muscle passes into the iliotibial tract, strengthening the lateral edge of the knee joint and strengthening the peroneal ligament.
In each section, it is not by chance that we are talking about the distal attachment points of the muscles surrounding the knee joint, because we are talking about the knee. Therefore, it is important to have an idea of which muscles surround the knee and are responsible for the various movements here.
During rehabilitation and therapeutic measures aimed at eliminating the consequences of knee injuries, it should be remembered that, by working hard, the muscles pass through themselves increased volumes of blood, which means oxygen and nutrients. This, in turn, leads to the enrichment of the joints with them.
There are two more large muscle groups, without which it is impossible to talk about the condition of the knee joints. These are the calf muscles, which are divided into anterior and posterior groups. The posterior group is represented by the triceps muscle of the lower leg, consisting of the gastrocnemius and soleus muscles. This "set" of muscles is responsible for the ankle extension and knee flexion. Accordingly, we can use the indicated muscle composition for the treatment of knee joint diseases.
The anterior group is represented primarily by the tibialis anterior muscle. Its function is to extend the foot, that is, to move the foot towards itself. It actively participates in the formation of the arches of the foot, with insufficient development of the tibial muscle, flat feet are formed. It, in turn, changes the gait in such a way that the load on the knee joints increases, which leads first to chronic pain in the knee joints, then to arthrosis of the knee joints.
Types of knee injuries
Possible knee injuries include the following:
Injury
Contusion is the most harmless possible knee injury. It is obtained by direct contact of the joint with any hard surface. Simply put, it is necessary to hit something.
Clinical signs of injury are acute pain that occurs immediately after the injury itself, gradually turning into aching, low-intensity, but very intrusive.
As a rule, pain in the area of the joint with injury is constantly present, it may increase somewhat with movement. The range of active movements is somewhat limited: extension of the joint is usually the most difficult. An exception is a bruise of the popliteal fossa, in which flexion of the lower leg can also be difficult. With this type of injury, the last few degrees of flexion of the leg at the knee are impossible not so much because of pain, but because of the sensation of a “foreign body” or a feeling of “jamming”.
The bruise passes on its own and does not need specific treatment, however, recovery can be accelerated in the following way:
- immediately after the injury, apply ice to the injury site;
- massage the joint area;
- do physiotherapy, such as magnetotherapy and UHF (on the 2-3rd day from the moment of injury);
- perform special exercises.

© PORNCHAI SODA - stock.adobe.com
Patella fracture
This is a much more serious injury than a bruise. It also involves direct contact of the knee joint with a hard surface. The blow, as a rule, falls directly into the area of the patella. This can be during jumping exercises (falling from a box for jumping, goat, parallel bars), when practicing contact martial arts or playing sports (hockey, rugby, basketball, karate).
In strength sports, such an injury can be caused by the lack of balance skills while holding the weight above the head, or the full extension of the leg at the knee joint under a critical weight (push, snatch, barbell squat).

© Aksana - stock.adobe.com
Signs of a patellar fracture
At the time of injury, a sharp pain occurs. The joint area along the anterior surface is deformed. Palpation of the patella area is very painful: in other words, you cannot touch the knee cup without severe pain.
Resting on the knee is possible, but very painful, as well as the process of walking. The joint is swollen, enlarged, the skin changes color. A hematoma forms at the site of the injury.
In the joint itself, as a rule, a significant hematoma is always formed with the occurrence of hemarthrosis (this is when blood accumulates in the joint cavity). The blood, in most cases, fills the joint cavity and some turns of the synovial membrane (see the Anatomy section). Purely mechanically, it exerts pressure on the capsule apparatus of the joint. In addition, liquid blood is irritating to the synovial interstitial space. These two factors mutually reinforce each other, leading to excessive pain in the knee joint.
Active and passive (when someone else is trying to extend your knee joint) knee extension is painful. With anesthesia under the skin, you can feel the patella, which can be displaced, deformed, or split. Depending on the tactics chosen by the traumatologist, treatment can be conservative or through surgical intervention.

© Snowlemon - stock.adobe.com
Treatment sequence for patellar injury
The sequence of actions will look like this:
- making an accurate diagnosis using an ultrasound machine and X-ray;
- puncture of blood from the joint;
- surgical intervention (if necessary);
- fixation of the knee and ankle joints for 1-1.5 months;
- after removal of immobilization - a course of physiotherapy, physiotherapy exercises (see the section "Rehabilitation after trauma").
Damage to the meniscus
In principle, any of the ligaments listed in the Anatomy section can rupture. However, the cruciate ligaments and menisci are most commonly injured. Consider first the damage to the menisci. (Learn more about knee ligament injuries.)
The role of the meniscus is to provide greater congruence of the articular surfaces and an even load on the tibial condyles. The meniscus rupture can be partial or complete. Simply put, the meniscus may simply "crack", which will violate its integrity, or a piece of the meniscus may come off.
The second variant of injury is less favorable - the detached cartilaginous fragment forms a chondral body that freely moves in the joint cavity, which, under certain conditions, can move in such a way that it will greatly impede active movements within the joint. Moreover, the chondral body can change its position several times without being in an “uncomfortable” state all the time. In this case, surgery may be required in order to remove the fractured fragment.
The variant with the formation of a meniscus defect is not so terrible. In such a situation, when performing certain therapeutic exercises, over time, the defect is completely "closed" by connective tissue.
The main problem with meniscus injuries is that if left untreated, over time they are more likely to lead to arthrosis of the knee joint, a degenerative disease that damages the cartilaginous component of the knee joint.

© joshya - stock.adobe.com
Cruciate ligament rupture
The front "crosses" are most often damaged. The load on them is greater even in everyday life, not to mention sports loads. This injury is common in short-distance runners, skaters, rugby players, basketball players, ice hockey players — all those who alternate periods of straight running with sprints. It is during the sprint, when the knee flexes and straightens in amplitude under significant load, that the cruciate ligaments are most easily injured.
Another option is to press the platform with overweight legs against the background of hyperextension of the knees at the final point of the press. The pain at the moment of injury is so strong that it can reflexively provoke an attack of nausea and vomiting. Lean support is very painful. No sense of stability when walking.
In the damaged leg, passive displacement of the lower leg with hyperextension of the knee joint is possible. As a rule, right at the moment of injury you are unlikely to be able to diagnose any specific damage. In any case, you will see spasmodic muscles around the joint, difficulty in active movement, and an increase in joint volume, most likely caused by hemarthrosis.
Treatment of damage to the ligamentous apparatus can be both operative and conservative. Plus operations in a speedy recovery. However, the operation can become a trigger for the subsequent formation of arthrosis of the knee joint, therefore, you should carefully listen to the attending physician and take into account his opinion regarding your case.

© Aksana - stock.adobe.com
Injury crossfit exercises
The most dangerous crossfit exercises for knee joints are:
- jumping onto a box;
- squats with full extension of the knee joints at the top;
- weightlifting snatches and jerks;
- short distance running;
- jumping lunges with touching the knees of the floor.
The exercises listed above, by themselves, do not cause knee injury. They can provoke it with an unreasonable approach to training. What does it mean?
- You do not need to dramatically increase your working weights and the number of repetitions. You do not need to work for a long time beyond the point of failure.
- You do not need to do this exercise if you have knee discomfort.
- At a minimum, you need to change the execution technique to the correct one, as a maximum - refuse to perform this exercise if it is not given to you in any way.
First aid
First aid for any knee injury is to minimize the build-up of hematoma and reduce pain. The simplest thing to do is to apply a cold compress to the joint area.
The compress is applied in front of both sides of the joint. In no case should the popliteal fossa be cooled.This is dangerous and can lead to vasospasm of the main neurovascular bundle of the lower leg.
If the pain is severe, pain reliever should be given. Of course, it is necessary to call the ambulance team and transport the victim to the point of providing trauma care.
Treatment
Treatment of knee joints after injury can be both operative and conservative. Simply put, first they can operate, then immobilize the joint, or they can simply immobilize it. The tactics depend on the specific situation and the injury. In this case, one cannot give a single recommendation for everyone.
The sequence of treatment is determined by an orthopedic traumatologist.
Do not self-medicate! It can lead you to sad consequences in the form of arthrosis of the knee joint, chronic pain and mediated damage to the hip joint of the same name!
There is a specific feature of the treatment of ligament damage. Regardless of whether the operation was performed or not, after a period of immobilization, and sometimes instead of it, partial immobilization using a hinged orthosis is applied.

© belahoche - stock.adobe.com
Rehabilitation after injury
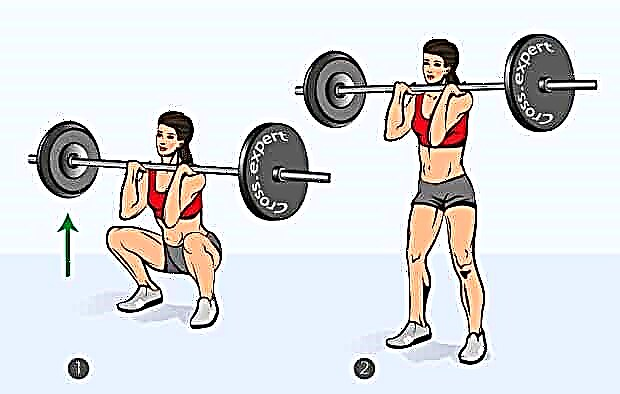
In order to strengthen the knee joint after injury, it is necessary to remove compression movements for a long period of time (up to a year). These are all types of squats, regardless of whether they are performed in the machine or not.
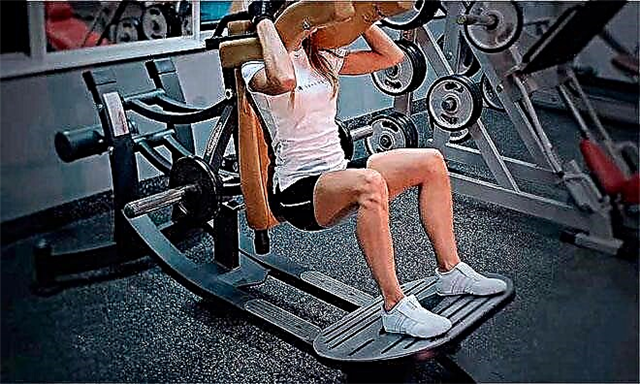
It is also necessary to strengthen those muscles that surround the knee joint: extensors, flexors, abductors and adductors of the thighs. The easiest way to do this is using specialized strength training equipment. Each movement should be performed at least 20-25 times. Breathing should be even and rhythmic: exhale for effort, inhale for relaxation. Breathe preferably with the stomach.
The complex should include the sequential execution of each of the above movements in one approach, with a weight that allows you to perform the specified range of repetitions.
Take the pace of execution slow, for two or three counts. The amplitude, if possible, should be maximum. In total, you can repeat up to 5-6 such circles per workout. As for the calf muscles, it will be helpful to do this: after each exercise that is not aimed at the muscles of the thigh, do the calf raises. Do this also quite slowly, with maximum amplitude and without holding your breath, until you feel a strong burning sensation in the target muscle group.
Start your rehabilitation course with one lap per workout and one set of calf raises.
By the end of the third month of rehabilitation, you should be doing at least 4 circles per workout and at least 2 times a week. From this period, with a favorable course of the rehabilitation process and the passage of pain, you can gradually return to compression loads. It's better to start with leg presses in the simulator with the development of your own weight. Only after that you can proceed to doing squats with their own weight.
However, all these moments are very individual! Listen to your body. If you feel uncomfortable, prolong the “no-compression” stage for some more time. Remember, no one except you at this stage will be able to determine the adequacy of the loads.