Bursitis (from the Latin "bursa" - a bag) - an acute or chronic inflammation of the synovial bag. Sources of the disease can be a blow, a fall, a heavy load on the joint, infection, wounds, and cuts. Timely diagnosis and treatment will usually lead to complete recovery.
General information
The bursa (bursa) is a fluid-filled sac-like cavity that is located around the joints and tendons, it is needed to cushion the tissues of friction during movement. There are about 150 of them in the body. They amortize, lubricate the joints between bones, tendons, muscles at the joints.
The synovial cells lining the bursal cavity produce a special lubricant. It reduces friction between tissues and the person can move easily.
With inflammation of the synovial bag, the release of joint fluid is reduced and pain, stiffness of movement, and redness of the skin appear. Distinguish between acute, subacute, chronic bursitis. The causative agent is specific and non-specific. The inflammatory process leads to the accumulation of exudate. By its nature, it is classified - serous, purulent, hemorrhagic.
With bursitis of the hip joint, the inflammatory process covers its synovial bag. Women of middle and old age are often susceptible to the disease.
The causes of the disease are usually:
- different leg lengths;
- surgical intervention;
- rheumatoid arthritis;
- scoliosis, arthritis, arthrosis of the lumbar spine;
- "Bone spurs" (processes on the surface of bones);
- hormonal disbalance;
- displacement of the head of the joint;
- dehydration of the body;
- ankylosing spondylitis;
- allergy;
- viral infections;
- salt deposits.
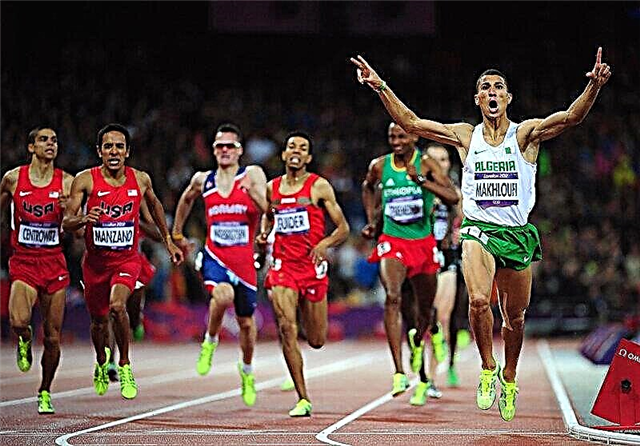
With intense jogging, cycling, frequent climbing stairs, or standing, there is an excessive load on the hip joint, which can lead to illness.
Symptoms
Against the background of general malaise, weakness appear:
- acute pain and burning sensation from the outside or inside of the thigh, radiating to the groin, pelvis;
- swelling of a rounded shape with a diameter of 10 cm;
- swelling of tissues;
- increased body temperature;
- redness of the skin.
Due to inflammation, a person cannot bend, straighten the hip. The pain is strong at first, but if you do not start treatment, it becomes weaker over time and the process becomes chronic.

© Aksana - stock.adobe.com
Kinds
Near the hip joint, there are the ilio-scallop, ischial, trochanteric cavities with fluid:
- Serpentine. More common than others. Pain appears in the area of the bony eminence on the lateral surface of the femur and adjoining tendons and ligaments. The patient experiences swelling, discomfort when moving, fever, weakness. At rest, the pain subsides, but when the person tries to climb the stairs, do the squatting - it intensifies. Even at night, if he lies on the affected side, he is worried about pain. It often manifests itself in women, the reasons may be excessive physical activity, excess weight, endocrine system diseases, osteoporosis, hip injuries, colds, viruses.
- Ilium-scallop (bone). It is characterized by inflammation of the synovial cavity located inside the thigh. Persons leading a sedentary lifestyle are at risk. It manifests itself as painful sensations in the groin, inner thigh, especially when trying to get up, sit down, raise a leg. Suffering intensifies after rest, sleep, immobility, when trying to get up, raise the hip.
- Ischio-gluteal. It is located at the point of attachment of the muscles of the back of the thigh to the ischial tubercle. The patient experiences pain in the buttocks, which becomes worse if he sits on a chair, flexes the hip, and lies on the affected side. The ischio-gluteal tuber increases. The unpleasant sensations are worse at night.
Diagnostics
The orthopedic doctor listens to complaints, examines the affected area, makes palpation. He makes a diagnosis using Aubert's test - the patient is placed on a healthy side and offered several movements - to withdraw, lead, raise, lower the hip. If he cannot fully do them, then the cause of the disease is bursitis.
In some cases, he prescribes MRI, X-rays, blood tests. Then, upon confirmation of the diagnosis, he recommends treatment.
Treatment
Bursitis is treated in a comprehensive manner. This is the intake of medicines inside, injections, external agents and physiotherapy.

Non-steroidal anti-inflammatory drugs (Ibuprofen, Indomethacin, Meloxicam, Celecoxib, Piroxicam, Diclofenac) help. They reduce pain and inflammation. Hormonal substances are used (Prednisolone, Hydrocortisone, Flosterone, Kenalog, Dexamethasone). Chondroprotectors (Dihydroquercetin plus, Osteo-Vit, Teraflex, Artra), vitamins, microelements are used. In advanced cases, antibiotics are prescribed (Cefazolin, Sumamed, Panklav).
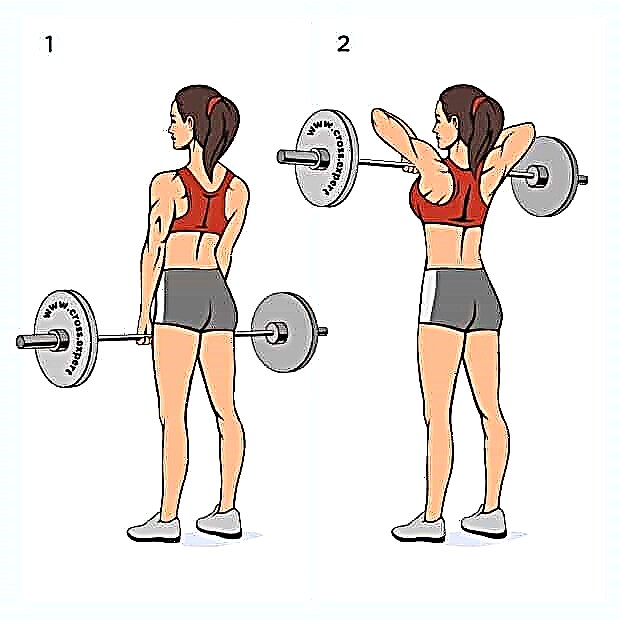
Physical activity is advised to limit, when walking, use a cane, crutches. Topically applied ointments - Cortomycetin, Nise, Dolgit, Voltaren. Additional measures - laser therapy, ultrasound, electrophoresis, inductotherapy, dry heat, paraffin applications, physiotherapy exercises, massage.

In advanced cases, surgical intervention is used - the excess fluid is pumped out under local anesthesia with a syringe.
The affected bursa is removed (bursectomy) in rare cases, when calcification occurs.
Traditional medicine uses herbal compresses - burdock, chamomile, yarrow, cabbage leaf and honey. Drink a drink made from honey and apple cider vinegar.
Consequences and forecast
In many cases, the disease is cured with timely referral to a specialist and early detection. There is every chance of recovery, movement is restored and pain disappears. But if the bursitis turns into purulent, a person can become disabled due to the destruction of cartilage tissue.
Complications in advanced cases can be - defects of the thigh, limited range of motion, venous insufficiency.
Prevention
To prevent illness, you need to not overload the joints, not carry heavy objects, use orthopedic shoes, control weight, and avoid injuries. Exercise in moderation, do stretching exercises and strengthen your thigh muscles. Do not forget about rest and good sleep, eat right, excluding harmful products, give up smoking and alcohol.